Laboratory Diagnosis of Pulmonary Tuberculosis
Describe briefly the laboratory diagnosis of pulmonary tuberculosis.
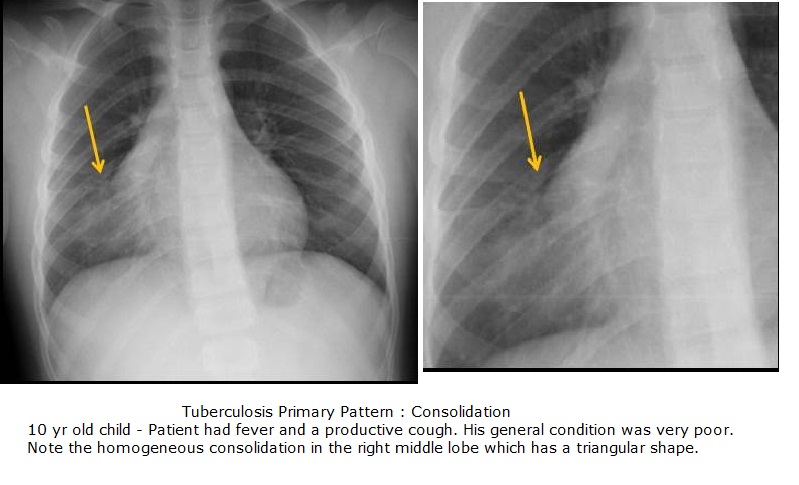
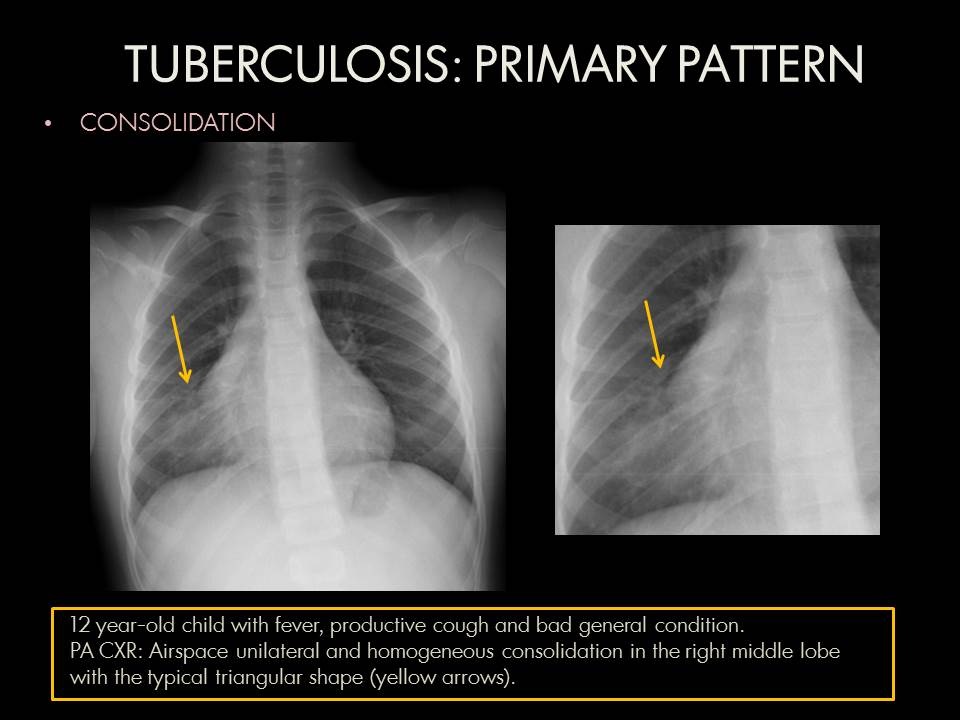
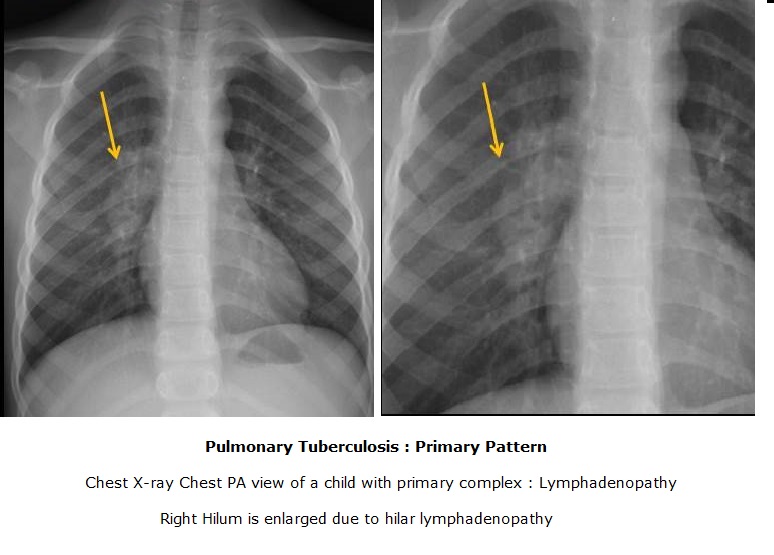
Radiologic Study
X-ray chest
Heterogeneous, often cavitary opacity in the apical and posterior segments of the upper lobes and the superior segments of the lower lobes. Cavitation
Patchy, poorly defined consolidation in the apical and posterior segments of the upper lobes and in the superior segment of the lower lobe is Radiographic stability for 6 monts and negative sputum cultures → inactive disease called radiographically stable TB, viable bacilli may persist
Post-primary TB heals with parenchymal scarring and nodules.
CT Chest
To detect fine lesions
To evaluate complications.
To detect bacterial activity.
Branching opacities, cavitation, or consolidation are clear signs of active TB,
"tree-in-bud" pattern, consisteing of multiple branching linear structures that represent bronchogenic dissemination of disease with caseating necrosis
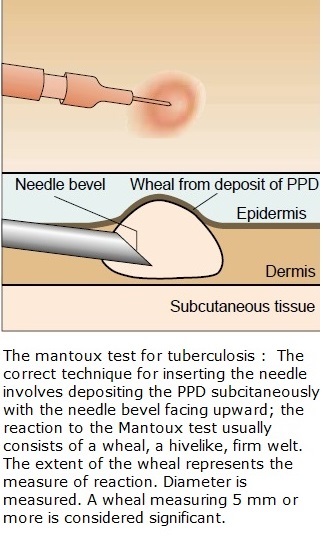
Mantoux Test
Tuberculin skin test
The Mantoux test / tuberculin sensitivity test / PPD test / purified protein derivative test is a tool for screening for tuberculosis (TB) and for tuberculosis diagnosis
A standard dose of 5 tuberculin units (TU - 0.1 ml) is injected intradermally and read 48 to 72 hours later.
A person who has been exposed to the bacteria has an immune response in the skin containing the bacterial proteins.
The response is a delayed-type hypersensitivity reaction - a type IV of hypersensitivities.
T cells and myeloid cells are attracted to the site of reaction in the timeframe of 1-3 days and generate local inflammation.
The reaction is read by measuring the diameter of induration (palpable raised, hardened area) across the forearm (perpendicular to the long axis) in millimeters. If there is no induration: "0 mm".
Erythema (redness) should not be measured
5 mm or more is positive in
An HIV-positive person
Persons with recent contacts with a TB patient
Persons with nodular or fibrotic changes on chest X-ray consistent with old healed TB
Patients with organ transplants, and other immunosuppressed patients
10 mm or more is positive in
Recent arrivals (less than five years) from high-prevalence countries
Injection drug users
Residents and employees of high-risk congregate settings (e.g., prisons, nursing homes, hospitals, homeless shelters, etc.)
Mycobacteriology lab personnel
Persons with clinical conditions that place them at high risk (e.g., diabetes, prolonged corticosteroid therapy, leukemia, end-stage renal disease, chronic malabsorption syndromes, low body weight, etc.)
Children less than four years of age, or children and adolescents exposed to adults in high-risk categories
15 mm or more is positive in
Persons with no known risk factors for TB
A tuberculin test conversion is defined as an increase of 10 mm or more within a two-year period, regardless of age. Alternative criteria include increases of 6, 12, 15 or 18 mm.
AFB smear microscopy and culture
Sputum is the most critical sample for laboratory testing.
Direct sputum smear microscopy is the most widely used method for diagnosing pulmonary TB
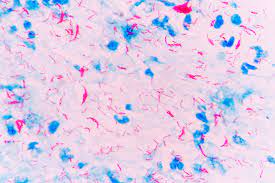
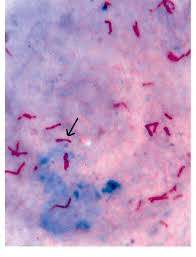
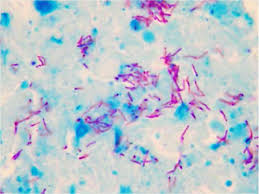
Conventional light microscopy of Ziehl-Neelsen-stained smears prepared directly from sputum specimens
Ziel-Neelsen microscopy is highly specific
Conventional fluorescence microscopy is more sensitive
LED microscopy
Culture of the bacteria on Lowenstein-Jensen slope or in broth media
Liquid media gold standard for initial isolation
ALS Assay
(Antibodies from Lymphocyte Secretions)
Antibodies from Lymphocyte Secretion or Antibody in Lymphocyte Supernatant or ALS Assay is an immunological assay to detect active disease
antibody from in vivo activated plasma B cells found in blood circulation for a short period of time in response to TB-antigens during active TB infection
Transdermal Patch
A similar approach to the ALS assay.
The transdermal patch is a method of detecting active M.tuberculosis circulating within blood vessels of patient.
This skin patch contains antibodies recognizing the secreted bacterial protein MPB-64 passing through the blood capillaries of the skin
Molecular methods
1) Nucleic acid amplification testing
Nucleic acid amplification (NAA) tests are a reliable way to increase the specificity of diagnosis,.
Drug Resistance
The initial M. tuberculosis isolate tested for drug resistance to ensure effective treatment.
Drug susceptibility patterns should be repeated when there is inadequate response to treatment;
When there is positive culture results despite 3 months of therapy.
Xpert MTB/RIF (Cepheid)
The Xpert MTB/RIF assay is a novel, rapid, automated, and cartridge-based NAA test that can detect TB along with rifampicin resistance directly from sputum within 2 hours of collection31. The GeneXpert cartridges are pre-loaded with all of the necessary reagents
Xpert MTB/RIF test
highly sensitive, and specific new tool for early TB detection and for determining rifampicin resistance.
A high proportion of rifampicin resistance is associated with concurrent resistance to isoniazid (~95%). Thus, detecting resistance to rifampicin can be used as a marker for MDR-TB with a high level of accuracy
* * * * * * * *